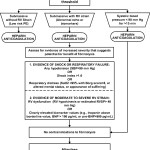
Definition of Massive PE-Acute PE with sustained hypotension (systolic blood pressure <90 mm Hg for at least 15 minutes or requiring inotropic support, not due to a cause other than PE, such as arrhythmia, hypovolemia, sepsis, or left ventricular [LV] dysfunction), pulselessness, or persistent profound bradycardia (heart rate <40 bpm with signs or symptoms of shock).
Definition of Submassive PE-Acute PE without systemic hypotension (systolic blood pressure >90 mm Hg) but with either RV dysfunction or myocardial necrosis.
- RV dysfunction means the presence of at least 1 of the following:
—RV dilation (apical 4-chamber RV diameter divided by LV diameter >0.9) or RV systolic dysfunction on echocardiography
—RV dilation (4-chamber RV diameter divided by LV diameter >0.9) on CT
—Elevation of BNP (>90 pg/mL)
—Elevation of N-terminal pro-BNP (>500 pg/mL); or
—Electrocardiographic changes (new complete or incomplete right bundle-branch block, anteroseptal ST elevation or depression, or anteroseptal T-wave inversion)
- Myocardial necrosis is defined as either of the following:
Fibrinolysis is reasonable for pts with massive PE and acceptable risk of bleeding complications (IIa/B)
Fibrinolysis may be considered for pts with submassive PE judged to have clinical evidence of adverse prognosis (hemodynamic instability, worsening resp. insufficiency, severe RV dysfunction, or major myocardial necrosis) and low risk of bleeding complications (IIb/C)
Fibrinolysis is not recommended for patients with submassive PE with only mild dysfunction, i.e. low risk PEs (III/B)
Fibrinolysis is not recommended for undifferentiated cardiac arrest (III/B)